May 28, 2017 marked the 15th anniversary of the law legalizing euthanasia in Belgium. According to the official data from their Federal Control Commission, euthanasia was performed on 14,753 individuals between 2002 and 2016.
The objective of this publication is to address the multiple issues raised by this significant number:
- the relevant law governing euthanasia
- the current debates to extend euthanasia
- specific statistical data
- cases of abusing the euthanasia law
- reactions to ethical abuse
I – SUMMARY
In 2002 Belgium decriminalized euthanasia for adults. By 2014, the law was extended to minors without specifying an age limit. For the past 15 years, the number of euthanasia cases has continued to sharply increase. Various modifications of the law have extended and facilitated euthanasia.
Several multi-faceted instances of abuse in interpreting and applying the law have been revealed by the available data. Numerous clandestine euthanasia cases continue to be practiced; the criteria to be respected have been incrementally subjected to broader interpretation (especially concerning the nature of “constant, unbearable and unrelievable physical or mental suffering”); as well as: the controversial role of the Federal Control Commission, the progression toward highly publicized assisted suicide cases; organ procurement after euthanasia; plus the pressure to eliminate the conscience clause, etc.
Especially in the Dutch-speaking regions, mentalities are rapidly evolving towards trivializing euthanasia, in the name of human autonomy and “one’s freedom to choose in favor of one’s own life or death”, via an Anglo-Saxon utilitarian perspective of life. Euthanasia is progressively being considered as a right that one can claim for oneself or loved ones, even if the prerequisite conditions are obviously not met.
Nevertheless, confronted with this exaggerated abuse, a genuine opposition has begun to speak out. For example: health professionals have testified to wrong-doings in their department, several films and documentaries have specified the conditions for euthanasia, religious representative have come together to defend the dignity of vulnerable individuals, without mentioning social media which continues to inform and alert on an international level.
II – STATISTICAL DATA
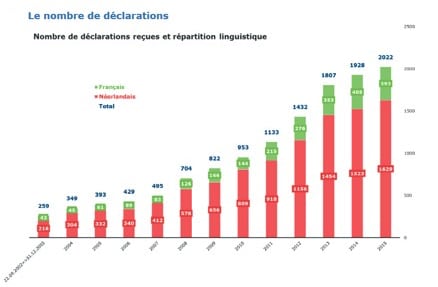
The Belgian Federal Control Commission received 2024 declarations of euthanasia in 2016, compared to 953 in 2010, thus more than doubling the rate in 6 years time.
The reality is even worse since these official numbers don’t account for numerous cases of clandestine euthanasia: estimated at 27% of the total cases in Flanders and 42% in Wallonia (cf § IV-2).
Therefore in Belgium there are approximately 6 « legal » euthanasia cases per day (for a population of 11.3 million, which is less than the Greater Paris region.)
More detailed statistics by region and by pathology are available in the Federal Control Commission’s report. More than 80% of the euthanasia acts took place in Flanders. The latest report published in October 2016 by the Commission includes data for 2014 -2015 (see Summary Table below and page 14).
Titles on the bar chart:
Number of declarations
Declarations by language: French, Dutch, Total
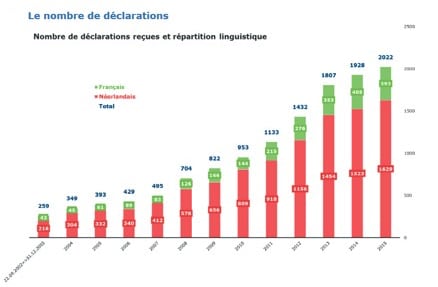
The European Bioethics Institute published a summary with a pertinent analysis and a bar chart.
III – LEGAL ASPECTS
1 - The original law of 2002
Euthanasia was decriminalized under certain conditions by the law passed on May 28, 2002. The text specified that doctors who “intentionally end the life of an individual who specifically requested” are to be exonerated from any responsibility if certain basic conditions and procedures coincide. The law (before it being extended to minors) includes the following key provisions:
- The patient is an “adult or an emancipated minor, capable and conscious, and thus competent to express his free will”.
- The doctor must verify that the patient personally makes the request “voluntarily and persistently, after careful consideration and is not a result of outside pressure”.
- The patient must have « a hopeless medical condition, be experiencing constant and unbearable physical or mental suffering which cannot be relieved, and is caused by a serious or incurable injury or pathological condition”.
- The doctor must consult a second practitioner to verify that all these conditions are fulfilled. If the patient is not in the terminal stage of illness, a third doctor must be consulted, either a psychiatrist, or a specialist for the patient’s pathology, and an additional one-month delay must be respected before the act can be performed.
- Once euthanasia has been performed, the doctor completes a form in order to ascertain the legality of the act performed. Doctors may invoke the conscience clause if they do not wish to perform euthanasia.
- Only a doctor may practice euthanasia. Some procedures called “preparatory, for example placing an intravenous line, are not part of the euthanasia practice itself”, and can thus be carried out by a nurse. Nevertheless, a nurse can also refuse to insert the perfusion (and as a general rule, no individual can be obliged to participate in performing euthanasia.
2 - The 28 February 2014 law for minors
In November 2013, the Belgian Senate proposed extending the 2002 euthanasia law for minors regardless of their age. This text goes beyond the limits of the Dutch law, which allows euthanasia for minors from age 12 and onwards.
This very sensitive subject was not thoroughly assessed at the House of Representatives (the equivalent of the French National Assembly). Those promoting the text aimed to have the bill passed very hastily. Thus on February 14, 2014 the Deputies voted in favor of the proposed text, which was legalized on February 28, 2014.
Belgium is thus the only country in the world which allows euthanasia to be practiced on children of any age, only on the basis of the child’s capacity of discernment, an element that is especially difficult to measure.
Certain specific criteria are required before practicing euthanasia on a minor:
- The minor must « be capable of discerning ».
- The patient must have “a hopeless medical condition, be experiencing constant and unbearable physical suffering which cannot be relieved, with a short life expectancy due to a serious or incurable injury or pathological condition”.
- He must be evaluated by a pediatric psychiatrist or psychologist, specifying the reasons for the medical appointment.
- The legal guardians (usually the parents) must sign a written consent form.
The doctors favorable for passing this law had estimated that a dozen youngs would request the procedure each year, however no requests for euthanasia of minors were recorded for over 2 ½ years. The first case was publically announced on September 17, 2016, by the president of the Control Commission, Professor Wim Distelmans, who had lobbied to have the law enacted.
3 - Draft bills for extending euthanasia
Since 2002, more than 20 draft bills have been submitted to the Parliament, mostly to extend euthanasia to other categories of individuals or to simplify the legal process.
The three most symbolic draft bills were submitted to the House of Representatives by the Deputy Onkelinx. These bills aim to modify advance declaration, the time span for the medical conclusion and the conscience clause.
- The first draft bill aims to «remove 5-year validity for advance declaration by letting the patient set the validity time limits himself.” Currently these advance declaration (similar to the French one, but focused on the individual’s request for euthanasia “in cases where the patient cannot express his will”), leaving the decision to the medical power of attorney that has been previously been personally named by the patient in his advance declaration.
- The second draft bill intends to reduce the medical delay for doctors to invoke the conscience clause: “the refusal must be given within 7 days of the request” and “the file must be transferred within 4 days of the refusal”. Currently, the law specifies that the consulting doctor who declines to perform euthanasia must inform the patient “in a timely manner”, and there is no formal time limit for transferring his medical file.
- The third draft bill aims to restrict the conscience clause, whereby no establishment can refuse for a doctor to perform euthanasia on its premises; as this would deprive “the practitioner from exercising his subjective freedom of conscience”. About this proposition, a trial was filed in May 2016 against the retirement home, Sint Augustinus, in Diest, the Flemish Brabant region, for its’ refusal to practice on-site euthanasia in 2011. After the family filed a legal complaint, the Louvain court issued the retirement home a 6000 € fine to pay family members for the detriment suffered for the inconvenience of transferring their mother to her domicile for euthanasia.
4 - A draft bill on palliative care during the examination
A draft bill to broaden access to palliative care was submitted on April 29, 2015. After being adopted by the Health Commission at the House of Representative on June, 7, 2016, it is currently being examined. It “seeks to widen the existing definition of palliative care for it to be better incorporated into the healthcare system” in order “that palliative care not only be limited to patients at the end-of-life”.
5 – A draft bill to change the legal definition of euthanasia as part of healthcare
Maggie De Block, the Belgian Minister of Social Affairs and Public Health proposed modifying the May 10, 2015 law entitled “Coordinated law for the practice of healthcare by professionals”, in order to include practicing euthanasia in the definition of a healthcare procedure (as one of the services offered by a professional practitioner but without a therapeutic or diagnostic objective).
On the one hand, this modification would lead to reinforcing the “cultural integration” of euthanasia in Belgium, and thus it could be considered as a medical or healthcare procedure.
On the other hand, this would elevate euthanasia to the status of « a right » in the broadest sense. “The euthanasia law” in Belgium remains a decriminalized law, meaning that any practice of euthanasia is punishable under criminal law, unless it is practiced under the strict legal specifications (cf § III-1). However, if defined as a healthcare procedure, euthanasia would become a right which the parents could request, with widely extended criteria for its application. Modifying its status would also substantially restrict the grounds whereby doctors can invoke the conscience clause.
IV – ABUSE RELATED TO NON-COMPLIANCE WITH LEGAL REQUIREMENTS
Several worrisome factors concern non-compliance with legal requirements.
1 - The debatable role of the Federal Control Commission
The Federal Control Commission has examined all the declarations submitted since the law was first passed in 2002. Until 2015, no cases were reported to the procurer, which casts a serious doubt on the commission’s impartiality. A significant number of its members advocate euthanasia, including the president of the Belgian association, the Right to Die in Dignity.
For the first time, on October 27, 2015, after having practiced euthanasia for 13 years and having examined 8000 cases, the Federal Commission submitted a file to the Court. It was Simona De Moor’s assisted-suicide case by Dr. Marc Van Hoeys, President of RWS “Recht op Waardig Sterven” a partner association for Right to Die in Dignity. This 85-year-old lady, Simona, complained of experiencing “inconsolable grief” following her daughter’s death. It is likely that the media coverage for the film “Allow me to die” may have encouraged the family to file suit. According to Le Soir website, Simona’s doctor insists that she “doesn’t want to die because she is depressive. No. But because she has had enough”. In addition, when the patient is not faced with an imminent death, a third doctor must be consulted, a regulatory compliance which was not respected in her case.
This Federal Commission, perceived by an increasing number of observers as a mere rubber stamping registration office, has ended up having its role and purpose challenged, to the point of being declared as a failure, and has been unable to recruit the necessary members, as it was the case at the end of 2015.
In an editorial published at the end of 2016, a group of ethicists and physicians deemed that the Federal Commission “unduly plays the role of a court”, by interpreting the law’s application in a “flexible” manner. Two examples were cited: that of assisted suicide, banned by law, but endorsed by the Federal Commission, and that of practicing euthanasia when the patient loses consciousness prior to euthanasia.
In March 2017, during a debate concerning the latest report filed by the Federal Control Commission, several MP’s called for public discussion on the sense of the law. They queried several recurrent problems, including the effectiveness of the Federal Control Commission, the media coverage of certain cases, the increasing amalgam between euthanasia and assisted suicide. The members of the Federal Commission, who were present, supported this proposed assessment.
2 - Continued high incidence of hidden cases of euthanasia
The Commission even acknowledges that all suspicious cases of euthanasia are not declared. During the documentary “Complement d’enquête” (Further Investigation) broadcast on France 2 Television at the end of 2014, the Commission’s President, Professor Wim Distelmans declared: “All the cases declared are in compliance with the law. There may be some small procedural mistakes, but all cases abide by the law. Obviously, since physicians do not report suspicious cases, we cannot verify them.”
Commenting on the report published in 2015, the same president recognized that officially reported euthanasia cases only account for part of the total number of acts performed in Belgium. According to the site “7sur7”, he stated: “One should recall that the total number still remains unknown since all cases are not declared, rendering it impossible for us to have a real grasp on the issue”.
In the previously mentioned editorial at the end of 2016, the group of ethicists and physicians deplored this situation and criticized the Federal Commission, especially its lack of resolve to evaluate and fight against non-declared cases of euthanasia, as well as its silence regarding numerous cases of “terminal sedation” (with high doses of morphine and sedatives) which should be analyzed as euthanasia cases to be declared.
As an example, in July 2012, a study carried out by scientists at the Université Libre de Bruxelles and the Gand University was published in Social Science & Medicine. Their results for a comprehensive investigation based on survey of 480 doctors in Flanders and 305 in Wallonia revealed that the Control Commission only included 73% of euthanasia cases reported by doctors in Flanders and only 58% of those reported in Wallonia. In other words, 10 years after legalizing euthanasia, 27% of the cases in Flanders and 42% in Wallonia remained undeclared.
3 - Non-verified and non-respected procedures
The July 2012 study previously mentioned revealed that the legal requirement for the second medical consultation was not respected by 73% of the Flemish doctors and by 50% of the Walloon doctors.
Another major study carried out in 2009 by Professor Raphaël Cohen-Almagor from Hull University (UK), was published in the journal Issues in Law and Medicine. The study revealed several major difficulties, for example regarding the legal requirement for a second physician’s opinion: cases were reported where the doctor rendering his opinion by telephone without examining the patient. Doctors regularly call the same colleagues who are known for being amenable to euthanasia.
In 2012, the European Institute for Bioethics dedicated a major document to this issue, underlying the abuses observed by furnishing “euthanasia kits” sold in pharmacies. The doctor who performs euthanasia in the patient’s home must personally return the non-used surplus product to the pharmacy. In practice, the lethal substances are sometimes given to the family, and no control of returned surplus products is carried out, giving rise to the fear of unauthorized use of these products.
Recently the media cited an example of procedures which are not respected by the doctors. Tine Nys, 38 years-old, had euthanasia performed in April 2010 after a romantic break-up. In February 2016, her sisters pressed charges against the doctors for negligence. In an interview broadcast by channel “VRT”, they gave witness to the euthanasia procedure carried out at their sister’s home. The doctor “didn’t have the necessary material for the injection”, “he forgot the bandages”. According to the European Bioethics Institute, Tine’s euthanasia report was only reported to the Control Commission 2 months later, instead of within the required time limit of 4 days. The sisters decided to file a judicial complaint.
4 - Organ donation following euthanasia?
This represents a potential new risk for breaking the law, even when the legal conditions are respected. Faced with an insufficient supply of donors, Belgian surgeons wish to advocate this practice for euthanasia cases, in order to increase the availability of organs for transplants. On September 28 2012, a symposium entitled “Euthanasia and Organ Donation” was held in Brussels, initiated by the Belgian Transplant Society, LEIF and the “Maakbare Mens” association. By analyzing the data since 2005 they ascertained that 9 patients had accepted to donate organs. Some physicians want to encourage this practice, estimating that up to 10% of potential organ donations could be procured from euthanasia patients.
Highly publicized cases have illustrated a rising inclination towards so called “altruistic euthanasia”. In 2015, the debate was fueled by a Dutch man, when his liver, kidney and pancreas were procured following euthanasia in a hospital in the Netherlands. Faced with increasing demands for organ donations, the Maastricht University Medical Center and the Erasmus Medical Center compiled a manual to streamline the process: “Euthanasia – Organ Donation”. According to Professor Ysebaert, a Belgian doctor at Anvers Hospital quoted in La Libre: “Currently we don’t mention this option to patients since it could provoke an emotional shock”.
A recent study by Dr. Jan Bollen at the Maastricht University Medical Center emphasized that at least 10% of individuals undergoing euthanasia could have donated at least one organ, meaning as many as 684 organs could have been made available for donation in 2015. A specialist in intensive care in Brussels, Professor Jean-Louis Vincent, confirms that he encourages organ donations from individuals who are “practically brain dead” (where the person is not completely dead) since the quality of the organs would be better.
V – A BROAD INTERPRETATION OF THE LAW
1 – From euthanasia to assisted suicide
Belgian law does not require for an individual to be in the terminal phase of an incurable serious disease, or for the medical staff to carry out an objective examination of the patient. For the physicians practicing euthanasia, as for the National Control Commission, the subjective evaluation of suffering has progressively come to be the only criteria taken into account. This leaves the door wide open to broader interpretations and shocking violations, on behalf of respecting individual autonomy.
For example here are some recent cases which could qualify as “assisted suicide”. Nowadays they are easily accepted by the laxest Control Commission, whereas they would have been excluded according to the debates for the 2002 law:
- Eddy and Marc Verbessem, two 45-year old twin brothers, born deaf
Eddy and Marc Verbessem, two 45-year old twin brothers, born deaf and suffering from glaucoma which would eventually lead to blindness had euthanasia performed on December 14, 2012. The fear of blindness was considered as “unbearable mental suffering” thereby attributing legitimate access to euthanasia according to their attending physician.
- Ann G., 44 years old, suffering from anorexia
Ann G., 44 years old, suffering from anorexia for many years, and was sexually abused by her psychiatrist, had euthanasia performed at the end of 2012 after declaring to have “cancer in her head”, thereby qualifying as suffering deemed sufficient enough to allow euthanasia to be legally performed.
- An ill prison inmate, serving a long sentence
A prison inmate, serving a long sentence and very ill, had euthanasia practiced in September 2012. This was the first case of euthanasia for an inmate in Belgium. Since then, a dozen more inmates have filed requests for euthanasia. Since the first incident known as the « Van Den Bleeken » case in 2014, (c.f. §V-2, refer to references), where euthanasia was permitted before finding an alternative solution, the debate has veered back to the return of the death penalty under the label of voluntary death sentences “for humanitarian reasons”. At the time, the European Bioethics Institute emphasized “an enormous failure in Belgian psychiatry” and denounced the Belgian penitentiary system which introduced “an inverted system of the death penalty”.
- Christian de Duve, 95-year-old Nobel Prize winner
Christian de Duve, 95-year old Nobel Prize winner, died by euthanasia on May 4, 2013. His family stated that the famous scientist serenely prepared for the procedure after having a fainting at his home. Throughout the month preceding his death he wrote to his friends and previous co-workers, and his last act was to give an interview to be published after his death in a leading daily newspaper. This case is similar to that of the well-known writer, Hugo Claus, who also organized his euthanasia in a likewise manner in March 2008.
- Nathan Verhest, 44-year-old transgender person?
Nathan Verhest, 44 years old, “profited” from euthanasia on September 30, 2013, after an unsuccessful sex change operation. Born as a female, she was rejected by her parents who wanted another boy, in addition to their 3 other sons. Having dreamed of becoming male since adolescence, she followed many cumbersome treatments to achieve this objective. After the last unsuccessful operation, she attested “I abhorred my new body” and claimed being tormented by mental suffering in order to obtain permission to have euthanasia.
- Kevin Chalmet, fireman, in his 30’s
Kevin Chalmet, fireman, in his 30’s, chose to have euthanasia in 2014 “to move the controversial debate forward”. Suffering from a brain tumor, this Belgian man progressively lost his sense of taste, and smell… The fireman thus prepared his euthanasia down to the smallest details, visited his fellow firemen at the fire station, wrote letters on his considerations, and planned the day of his death. He attested: “Everything will take place at home but first we’ll have pastries.
- Johnny Vaes, 59-year-old man with pancreatic cancer
Johnny Vaes, 59-year-old man with pancreatic cancer, scheduled his euthanasia procedure for Friday May 13, 2016, after a final farewell to his loved ones. According to the web site “be”, this father had no hope of recovery once his cancer had metastasized. At that point, he had announced his upcoming euthanasia procedure on Facebook and invited his loved ones to the hospital for a last get-together. The man declared: “For lunch I’ve asked for French fries with mayonnaise and ketchup. Afterwards, I’ll have my shot, and I’ll leave.”
These highly publicized cases in the Belgian media, demonstrate a growing tendency to trivialize the act of euthanasia, and more recently the staging and dramatization of death.
2 – Mental suffering: where are the limits?
Increasing numbers of individuals (124 people in just two years 2014 and 2015) have been put to death by euthanasia for “mental illness and behavioral disorders” including people with depression, Alzheimer’s, dementia, etc. This worrisome trend was analyzed in an interview published by Atlantico in October 2016:“signifying that in spite of having altered mental faculties, doctors acquiesced to their request”.
Nevertheless, certain cases of euthanasia were avoided at the last moment, or may still be pending today. The following symbolic cases highlight the ambiguity of the situation:
- Laura Emily, 24 years old
Laura Emily, 24 years old. In 2015, “The “Economist” broadcast a documentary of Laura Emilie’s story entitled « 24 and ready to die » who remained alive after having requested euthanasia. Following a difficult childhood, and suffering from depression, she requested euthanasia on September 24, 2014. Three doctors accepted her request, justifying that she suffered from “incurable mental suffering” a condition allowed by Belgium’s 2002 euthanasia law. On the appointed day, with journalists present to film her death, at the last minute, Laura Emily refused and declared: “I can’t go through with it. These past 2 weeks were relatively tolerable; there were no crisis situations. It’s unclear for me: did something change inside me, or did something change so that things have become tolerable?” The young lady is still alive today.
- Franck Van Den Bleeken, prison inmate in his 50’s
Franck Van Den Bleeken, prison inmate in his 50’s, had been convicted of murder and several rapes and had already spent 30 years being incarcerated. Although he was in good physical health, Franck attested that he could no longer stand being in prison. The legal system in Belgium denied his transfer to a hospital in the Netherlands. He then requested euthanasia and obtained permission from the doctors treating him, by invoking “incurable mental suffering”. Following a widely publicized debate which accused the Belgian government of being unable to propose an adequate medical treatment, the doctors reversed their decision, and ended up transferring him to a specialized psychiatric clinic in Gand.
- Sébastien, 39 years old
Sébastien, 39 years old, sought euthanasia in March 2016, for his 40th birthday. During an interview for “20 minutes”, this pedophile explained: “I have been in therapy for 17 years. I spent 4 years in a psychiatric hospital. I’ve seen 8 psychologists, 4 psychiatrists, and a sexologist […] at this point, I don’t want anything”. To date, his request for euthanasia has not been authorized. According to the French television channel, France3, the psychiatrists estimate it will take 18 months before being able to verify the validity of his request.
3 – Growing pressure for economic reasons
In an article published on January 17, 2017, Dr. Marc Moens warned that “budgetary problems in healthcare for the elderly, may lead to debating euthanasia policies based on socio-economic reasons.” In various media and medical circles “there are open pleas in favor of euthanasia for Alzheimer patients” and demands to stop treating some incurable diseases, to invest healthcare money for patients with treatable conditions. However Dr Moens concludes: “Euthanasia should never become a cost-related solution. However, the “slippery slope” is dangerously close”.
ANNEX : INCREASING COMPLAINTS OF VIOLATIONS
Since euthanasia was legalized 14 years ago, there has not been any strong public criticism, and thus appears to have been progressively accepted. In 2014, Belgian public opinion was rather favorable to extending the law to minors. Recently, however, due to multiple abuses of the law, there have been increasing numbers of initiatives and protests both in Belgium and internationally, that challenge euthanasia as a routine practice.
1 - Protests by health professionals
- In June 2012, over 70 well-known figures, mainly health professionals signed a major text marking 10 years of euthanasia practice in Belgium. Their statement emphasized how this law, by opening “Pandora’s box” and transgressing the original founding prohibition, results in the public’s loss of trust, and in weakening individuals who are already the most vulnerable.
- In May 2013 an internet site euthanasiestop.be was created by doctors, professors and well-known Belgians to respond to draft bills aiming to extend euthanasia. This means of exchanging information is progressively creating public awareness.
- On February 12, 2014, over 172 pediatricians signed an open letter to the presidents of each of the Belgian political parties. At the time of the draft bill for extending euthanasia to minors, these professionals throughout Belgium considered that further discussion was needed. They emphasized the ambiguous terms in the draft bill: “In practice, there is no objective means to determine a child’s understanding and judgment. The assessment is widely subjective and prone to influence.”
- In September 2014, Corinne Von Oost, director of a Palliative Care department in Belgium, published a book entitled “Catholic Physician, why I practice euthanasia”. When interviewed by “La Croix” (The Cross) newspaper, she declared that practicing euthanasia doesn’t have any particular meaning for her: “it’s a way of responding to nonsense, by nonsense”, and admitted that “the danger is to become accustomed to it”. Retorts to this widely publicized work appeared rather quickly. In December 2014, Marie-Dominique Trébuchet, PhD in theology and volunteer for palliative care retorted in “La Croix”: “To answer Dr Van Oost’s question “Who am I to refuse to help someone die”, let’s ask ourselves “Who am I to put someone to death?” In January 2016, Catherine Dopchie, Catholic oncologist and director of an intensive care unit, also responded in “La Libre”: “The psycho-spiritual suffering of not finding any meaning in life, nowadays the root cause of most requests for euthanasia, is not a medical issue, strictly speaking.
- On September 10, 2015, a joint group of 38 university professors, psychiatrists and psychologists published in “Le Soir”. In their article, they expressed their serious concern due to the increasing number of euthanasia acts performed on individuals suffering from mental disorders. Referring to the case of Laura Emily, they emphasized that “experience confirms that the pertinent legal guidelines solely for mental reasons is questionable”. In fact, “unbearable mental suffering cannot be confirmed, since there are no measurable parameters, no tissue biopsy, nor any behavioral signs which can be objectively evaluated.”
2 - Increasing civic oppositions in society
- In September 2013, Professor Etienne Montero, dean at Namur University of Law, published a book: “Appointment with Death: 10 years of legal euthanasia in Belgium”. In his book, he gives a critical summary of the situation, underlining how legal guidelines are broadly interpreted, and warns of the “slippery slope” phenomenon: “The problem is that if the only criterion for euthanasia is based on an individual being able to give informed consent, Belgian law allows justifying euthanasia for almost any situation. The condition of suffering is subjective, and the concept of a serious illness is defined in various manners.”
- Pierre Barnérias, a French journalist, produced the film “Euthanasia: how far can we go?” which presented the violations of the law in Belgium. In October 2013, when interviewed by La Croix, he declared: “The main criticism is the lack of verification in spite of having a Federal Commission. Some of the witnesses, one of whom appears in the film, even accuse the practice as being homicides disguised as euthanasia!” Although his objective is not to take a position either for or against euthanasia, he nevertheless aims to demonstrate that in Belgium, “the practice of euthanasia is not free of abuses”.
- On November 6, 2013, the main religious figures in Belgium released a historical message. For the first time the 3 main monotheist religions, the representatives from Christianity (Catholics, Protestants, and Orthodox), Judaism, and Islam expressed their serious apprehension faced with the risk of trivializing euthanasia. They protested extending the law for minors or for dementia, because this would signify “an extreme contradiction to mankind’s existence” and concluded: “we cannot endorse this mentality which would lead to destroying society’s basic foundation”. The previous Finance Minister and head of the Flemish Christian Democratic Group (CD&V), Steven Vanackere called for a reevaluation of the law in February 2016. According to the Figaro newspaper, his intention was not to eliminate the law, but to “have the violations evaluated”. He also denounced the composition of the members in the Control Commission, because “there are members who perform euthanasia, representing a conflict of interest if they judge their own cases”. “We want to encourage a genuine social discussion, beyond ideology, and by involving the public. This kind of evaluation will certainly create public awareness of the transgressions of the law.” Since 2001 the European Institute of Bioethics (EIB) has been monitoring the changes in the legislation, practice and mentality in Belgium. For example in January 2013 when the twin brothers had euthanasia performed, one of the directors emphasized how this was downplayed by the Belgian public. “The list of incurable diseases is practically endless (…) The definition of psychological suffering is left to the subjective interpretation of the person concerned (…) Finally, the legal condition is practically customized to authorize euthanasia if there is voluntary and persistent request from anyone suffering diverse pains, solitude, or who is tired of living (…) We are already witnessing how euthanasia is being considered commonplace in Belgium”. In 2014, during the discussion for extending the law to minors, the European Institute of Bioethics warned “today the population is ready to accept a situation that was considered reprehensive 10 years earlier. It is impossible to deny the genuine trivialization of euthanasia and assisted suicide… Is this the manner that society wishes to relieve the distress and suffering of weak or ageing individuals who are sick or disabled?” On October 24, 2016, in a long interview with “Atlantico”, Carine Brochier gave an updated analysis of euthanasia violation, calling for a better accompaniment for the ageing rather than continually enlarging the legal criteria.
- More recently, on December 28, 2015, the new Belgian primate, Bishop Jozef De Kesel, was interviewed by the “Het Belang” He reaffirmed that healthcare institutions have the freedom to practice euthanasia or to refuse. One institution, in January 2016, refused to have euthanasia practiced on its grounds (c.f. §III-3). The cardinal declared: “I think that we have the right to decide as an institution whether or not to allow euthanasia. I am thinking of our institutions”.
3 - Des réactions internationales
- At the end of January 2014, 61 members from several different countries and political parties at the Parliamentary Assembly for the Council of Europe signed a declaration concerning a draft bill on euthanasia for Belgian children. This declaration especially noted that “euthanasia must remain prohibited whenever it consists of intentionally killing a dependant human being, presumably for his own interest, by an action or by an omission”. The European MP’s also remarked that Belgium “betrays its most vulnerable children by not attributing an intrinsic value to their lives”.
- On February 10-11, 2014, an International Congress for Pediatric Palliative Care was held in Mumbay, India. At that time, as many as 250 experts from 35 countries published a statement to warn Belgium against extending the 2002 law to minors. The final statement “urgently called for the Belgium government to reconsider its recent decision”. These physicians “demand that all children at the end-of-life have access to the appropriate means to alleviate their symptoms and their suffering, as well as high quality palliative care specific for their needs”. The statement added:” We don’t consider that euthanasia should be included as part of pediatric palliative therapy; it is definitely not an option”.
FOR FURTHER INFORMATION:
- Euthanasia: 10 years of practicing euthanasia in Belgium. A very complete report dated April 2012, from the European Institute of Bioethics, regarding legislation and practices, with concluding remarks on the lack of effective monitoring of the law’s application.
- CCNE Opinion N° 121 on the End-of-Life, dated July 1, 2013. Annex 2 summarizes assisted suicide and euthanasia experience abroad: analysis of Benelux countries pages 73-77.
- Federal Control Commission, Report 2014-2015, published in October 2016: Statistical Summary with detailed data of euthanasia procedures in 2014 and 2015.

![[Press Release] End-of-Life: Utmost Vigilance for Highly Dependent Patients](https://www.alliancevita.org/wp-content/uploads/2017/06/ConseilConstitutionnel.jpg)