Euthanasia and Assisted Suicide Abroad : Feedback of Experience
Feedback of experience on euthanasia and assisted suicide abroad
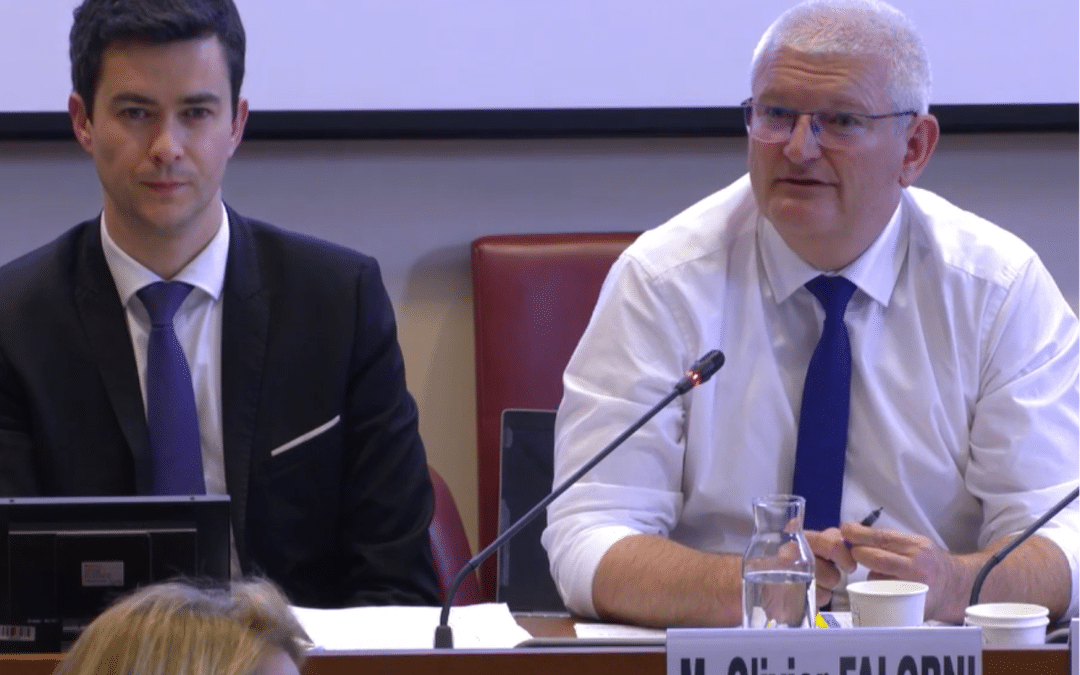
The contributions from the International Symposium on the end of life, organised by Alliance VITA in collaboration with the European Bioethics Institute (Belgium) and the Living with Dignity citizens’ network (Canada) were published on 22nd May 2024 in a common document.
The feedback of experience from five nations (Belgium, Holland, Switzerland, Canada and United States) who have authorised euthanasia or assisted suicide practices for several years, constitute a particularly pertinent statement in the context of the debate concerning the end-of-life bill in France.
The contributors are all experts in their nations. Some of them have been players in the establishment of such practices or were not in principle opposed to them.
During the symposium, the legal and medical impacts were considered, as well as the wider subject of the repercussions of assisted suicide and euthanasia on society itself.
I.The legal aspects
Whether in Holland, Belgium, Switzerland, Canada or Washington State (United States), the initial framework was intended to be strict. However, the original conditions were unable to stand fast anywhere.
- Extendable criteria
As years have passed, the criteria have been stretched by interpretation or legalisation under the influence of a double logic well described by Léopold Vanbellingen the Belgian lawyer: the logic of the subjectivity of suffering and the logic of non-discrimination have led to “an extension to cases which were quite unimaginable at the moment of adoption of the law”.
What patients say about suffering becomes law. Currently in Belgium, in Holland, in Canada and even in Switzerland – which accepts only assisted suicide – people suffering from depression, multiple pathologies associated with old age, are eligible for induced death. In Belgium as in Holland, even children can be euthanised.
In Holland, professor Theo Boer explains that the dynamics have become uncontrollable : “19% of the pathologies claimed when applying for euthanasia concern patients who are not in their terminal phase”. In Washington State, which has adopted similar legislation to that in Oregon, the screening for mental health problems, which is in fact mandatory in order to obtain a prescription for suicide products, is practically never undertaken, as stated by doctor Shane Macaulay.
- Ever increasing figures
From a hundred cases predicted in Quebec in 2015, there are now over 1000 cases of euthanasia per year a mere seven years later and over 13,000 in Canada as a whole. Quebec has become the world champion of euthanasia accounting for some 6.6% of deaths in 2022 ahead of Holland with 5.5%. In some regions in Holland, euthanasia represents 10 to 20% of deaths. In all nations, the graphs of deaths by euthanasia or by assisted suicide are climbing — without even considering persistent illegal euthanasia.
In order to cope with this increase, many requests are being made in Holland to alleviate the task of the supervisory commission which is overloaded. Some are suggesting using random checks or limiting checks to cases of dementia or psychiatric disorders.
Contrary to what some people thought, the acceptance of euthanasia or assisted suicide has not led to any fall in the number of suicides.
- A Canadian particularity: the term of “Medical Assistance in Dying” or MAiD
The term is a euphemism for euthanasia and assisted suicide. The expression contributes to the spreading of confusion concerning palliative care and even care in general, as was underlined by professor Trudo Lemmens. To the extent of presenting death as being a good thing, or even a kind of therapy.
- The “libertarian” downward slide of the law
Professor Lemmens has noted a trend which is not liberal but rather libertarian of the law which absolutises the choice of an individual at the expense of the true value of liberty. He challenges the question of choice when one cannot have access to healthcare: that is a major problem in Canada. For mental conditions, there is often a delay of several months before patients, even those showing suicidal tendencies, can obtain an appointment with a psychiatrist!
It can be seen that this liberty, which is presented as individual, is in fact authoritarian. In Belgium, the practice of euthanasia which initially was left as a free choice for institutions was made compulsory in 2021 for all old people’s homes and medico-social establishments. The same in Canada. In Switzerland, several cantons have also made compulsory the acceptance of suicide associations in old people’s homes on pain of losing their state subsidies.
II. At the medical level
- The difficult coexistence of palliative care with induced death
The prolonged experience of the coexistence between palliative care and the possibility of induced death shows that the two approaches are plainly incompatible.
That is the conclusion by the ex-president of the medical association for the State of Washington. The presence of professionals who are in favour of assisted suicide in healthcare establishments undermines the commitment to make full use of the potential of palliative care. Doctor Catherine Dopchie has observed in Belgium the diminishing research into palliative care to the benefit of proposing euthanasia in the planning of care.
In Canada, the supreme court suggested that one could use the opportunity of the legalisation of “medical assistance in dying” to reinforce the development of palliative care services, which were largely understaffed at the time of legalisation in 2016. Today, some 40% of people who are euthanised have little or no access to palliative care.
Doctor Leonie Herx, a Canadian doctor in palliative care, explains that requests for euthanasia take up the time of professionals, who are no longer able to provide appropriate care, to the extent that some of them even resign. Patients turn towards euthanasia at the suggestion of their doctor because “they fear that their symptoms will become very serious”.
- The deterioration of the carer-patient relationship
Although the conscience clause is vital, including for pharmacists, and is effective in all the nations represented, the professionals feel powerless in the face of requests for a programmed death.
According to doctor Catherine Dopchie, “This contract which you have to execute, seriously jeopardises the healthcare mission as well as the sheer resilience of patients”. The perceptible relinquishment of medicine experienced in a relational form constitutes a major challenge, revealed through the discussions at the carers’ round table. What is at stake when induced death becomes commonplace, whether by euthanasia or assisted suicide, is the loss of the human link.
Doctor Paul Lieverse, the Dutch specialist on pain, has learned over time that the very thought of euthanasia takes root in the fear of suffering and the fear of inadequate relief. His approach, based on listening to needs, has achieved the “evaporation” of many of the euthanasia requests which he has received. He is particularly concerned at the lack of training in palliative care for young doctors in Holland and the mutation of medical practices. He quotes the case of a woman suffering from Alzheimer’s who had asked for euthanasia through advance directives.
The woman struggled when it came to the injection of the lethal product: she was then put to sleep to be euthanised.
- The mishandling of suicide prevention
Whence the alerts by the professionals on suicide prevention. Johannes Irsiegler, a Swiss psychiatrist explains that there is no difference between motivations for suicide or for assisted suicide: the desire is not so much to no longer live but to not live under those circumstances. But in the case of assisted suicide, there is the involvement of a third party “the person is confirmed in her/his renouncement to live”.
III. On the social level
Some people consider that assisted suicide and euthanasia merely constitute a new individual right which takes nothing away from the person, which professor Theo Boer considers as “moral populism”. However, the example of foreign nations shows the significant impact which these practices exert on patients, their entourage, the carers, the more vulnerable and more generally on the way of apprehending death and human solidarity.
- Repercussions on family members
The statement by Canadian Laurence Godin-Tremblay bears witness to the violence which may be caused by the legal exclusion of the family from the decision on assisted suicide or euthanasia. A Swiss study has shown that 20% of family members experience post-traumatic stress and 16%, deep depression following an assisted suicide. Léopold Vanbellingen refers to what he calls a “spiral of silence” which may build-up within the entourage with the following subjacent question: “Who am I to question a request for euthanasia? ».
- A dangerous exposure of the most vulnerable
In 2021, the Canadian law deleted the requirement of a reasonably predictable death, which was already open to interpretation, and seriously damaged the consideration of the handicapped. According to professor Trudo Lemmens, the increase in numbers of applications for medical assistance in dying for socio-economic reasons, is an indication of the changes to society which go against social justice.
He questions the nature of intolerable suffering claimed in order to be entitled to medical assistance in dying. Signals “are indicating that people are dying for economic reasons “. He quotes the cases of handicapped people who say explicitly to their lawyers that they will apply for euthanasia if they fail to obtain aid.
- Gradual trivialization of administered death
Professor Theo Boer made a similar comment for Holland explaining that the way we consider “old-age, vulnerability, dependence on care and our very notion of humanity has changed”. Euthanasia has become a “normal” death for certain diseases (cancer, neurological disorders, dementia, psychiatric disorders etc.).
François Truffin, a Belgian nurse, explains that euthanasia has become a form of routine in the accompaniment for the end of life. Concerning the spiral effect, professor Theo Boer speaks of a “spiral of despair” which imprisons and causes a headlong rush. He quotes the current proposal for a law on the so-called “accomplished life”. He worries about the positive presentation of some forms of euthanasia for couples (together) in Holland as if our society had no other solution in the event of widowhood.
- Beware of the Werther effect or mimetic suicide
The warning by Stève Bobillier on the scientifically recognised phenomenon of mimetic suicide is particularly pertinent at a time when France intends to legalise assisted suicide. “If suicide is presented publicly as a possible way out, which is even boasted by some, if even celebrities choose it, then the most vulnerable, the aged, the sick, the young or those suffering from psychological difficulties, will consider it as the thing to do”.
Other questions were considered, such as organ donation following euthanasia or advertising for assisted suicide or euthanasia.
From this general presentation, readers are encouraged to take time to discover the wealth of each contribution punctuated with references and concrete situations as well as the three brief round tables. Assuredly “the democratic debate calls for enlightenment by what is actually happening” in order to legislate in full knowledge and without interfering with the difficult protection of the most vulnerable.