
Opposability of Advance Directives: The Limit Established in Law, Validated by the Constitutional Council
The Constitutional Council has been consulted in a conflict opposing the family of a patient and his medical team concerning the application of his advance directives.
A patient in an irreversible coma state (Abdelhami M., 43 years old), following an accident, had indicated, in writing, a desire to be kept alive whatever the cost if he ever found himself in such a situation. However, ten days after the accident, his medical team considered that the treatments keeping him alive artificially could be considered as unreasonable obstinacy. Judged to be futile and disproportionate, these heavy treatments, in their view constituted aggressive therapy. This is prohibited by the medical code of practice; as well as by law. But family members immediately referred to the courts, quoting his written wishes, to prevent the interruption of his life support. The case has been referred to the Constitutional Council.
The so-called Claeys-Leonetti law, dated 2nd February 2016, has reinforced advance directives. They are considered, in addition to the advice of the person of confidence, as a privileged expression of the will of a patient unable to express his/her wishes. In the case concerned, paragraph 3 of article 8 of the law was in question: “The advance directives are mandatory for the doctors for all investigation, operation or treatment decisions, except in the case of life-threatening urgency during the time necessary for a complete evaluation of the situation and when the advance directives appear manifestly inappropriate or non compliant with the medical situation.” The paragraph uses wording which could be considered ambiguous or even contradictory concerning the use of the term “mandatory” immediately combined with notable exceptions. It is the final part of these exceptions on which the Constitutional Council is being called upon to judge the validity, through a “Priority Ruling on Constitutionality”.
Which should take precedence between the opposable advance directives – or the collective decision by the doctors?
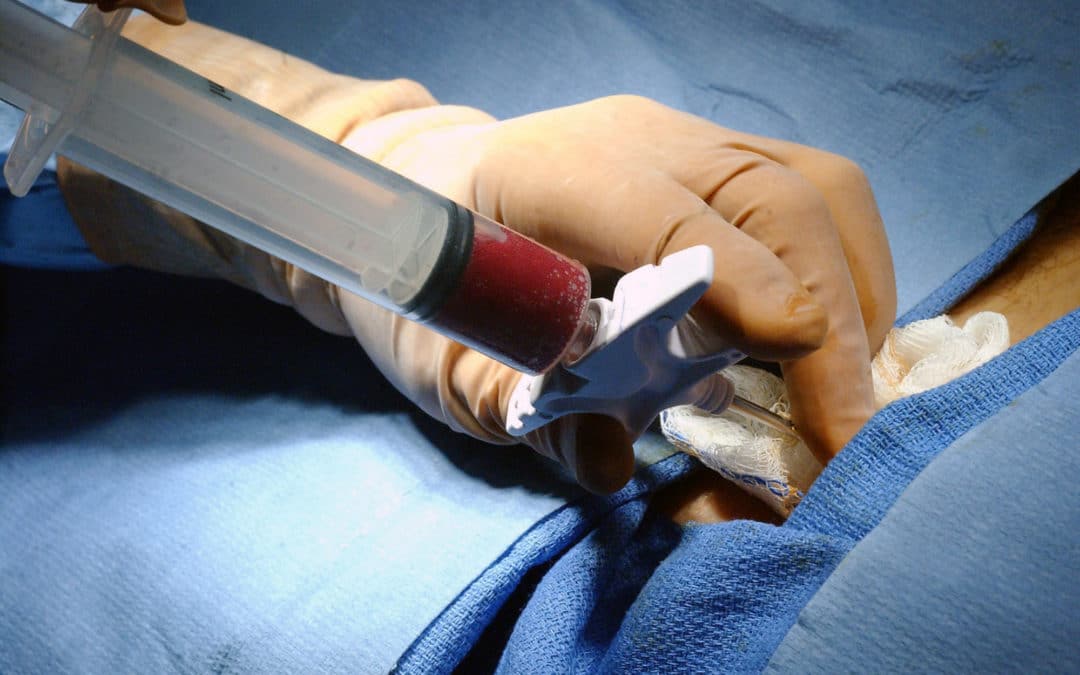
Unconscious, under artificial respiration, hydrated and fed artificially, benefiting from transfusions (a different situation from that of Vincent Lambert, who could breathe spontaneously and stably) his condition is judged to be both catastrophic and irreversible by the medical team. Their lawyer additionally notes that the artificial life-support for the patient is inevitably a heavy burden on the health system. He quotes in particular article 1111-11 paragraph 3 of the public health code (article 8 previously mentioned of the law) which is intended to attenuate the bearing of the advance directives since the doctors are no longer compelled to follow them when “they appear manifestly inappropriate or non compliant with the medical situation.“
In reviewing the 2005 end-of-life law, the legislator, whilst reinforcing the “opposable” nature of advance directives aimed at avoiding their abuse: making them truly opposable would make the patient his own prescriber and the doctor a mere executor of that prescription. Medical competence – the medical art – prohibits submitting doctors to the potentially excessive or medically unfounded requirements of patients or their family members. It is the doctors who in principle have the competence. The paragraph in question thus provides a means of resistance to possible prior requirements which are tantamount to demands for euthanasia, which is an illegal practice.
The decision by the Constitutional Council
Through this particular case, the Constitutional Council finally validated article 1111-11 paragraph 3 in its current wording, therefore including the limit which the legislator intended to introduce regarding the opposability of advance directives. The wording “when the advance directives appear manifestly inappropriate or non compliant with the medical situation” in the third paragraph of article L. 1111-11 of the public health code, in its wording resulting from ruling No. 2020-232 dated 11th March 2020 relative to the regulations governing decisions taken on matters of health, funding or social or medico-social accompaniment with respect to adults subject to legal protection measures, are compliant with the Constitution.”
More generally, the upholding of the paragraph confirms doctors in their authoritative role for the pursuit or otherwise of life support treatments. Implicitly, this case confirms that advance directives, although useful, are in no way a guarantee of a “good death” and that they are no guarantee either against conflicts. It should be added that it is not certain that a patient demanding in advance to be kept alive “at whatever the cost” has any enlightened conscience of what is being asked for. Constitutional Council indicated additionally that “by allowing doctors to go against advance directives the legislator considered that the latter could not be mandatory in all circumstances, inasmuch as they are prepared at a time when the person is not yet confronted with the particular end-of-life situation in which he/she will be unable to express his/her will due to the critical nature of their condition. Notwithstanding, he intended to guarantee the right of any person to receive the most appropriate treatment for their condition and ensure the safeguard of the dignity of persons at their end-of-life.”
By validating the current wording of this article, the Constitutional Council confirms the balanced nature of the text with regard to the constitutional principles in its care.



![[Press Release] – 2nd November: 10 Ideas from Alliance VITA for Solidarity and Against the Drift Towards Euthanasia](https://www.alliancevita.org/wp-content/uploads/2022/10/main-672x675.png)
![[Press Release] – 2nd November: 10 Ideas from Alliance VITA for Solidarity and Against the Drift Towards Euthanasia 1 10 idees](https://www.alliancevita.org/wp-content/uploads/2022/11/10-idees-300x293.png)